Stay ahead of the curve as a political insider with deep policy analysis, daily briefings and policy-shaping tools.
Request a DemoIndiana’s trauma care system falls short in rural counties; will money in the budget be enough?

Pulaski County EMS, which typically runs two ambulances across the county's 435 square miles of mostly farmland, is headquartered in Winamac, Indiana, Feb. 7, 2023. (Credit: Ryan Martin)
WINAMAC, Ind. — When it’s time to move a patient from this town’s six-bed emergency room to a larger hospital specializing in trauma care, Brandon DeLorenzo sometimes has to wait.
The Pulaski County emergency medical services director can typically spare one of his two ambulances to make the 1 hour and 15-minute drive to the nearest trauma centers in Lafayette or South Bend.
But occasionally when a medic takes a vacation, DeLorenzo is down to one truck — and he’s forced to keep it available for a potential vehicle crash or other emergency somewhere across the 435 square miles of mostly farmland.
So trauma patients wait at Pulaski Memorial Hospital for sometimes hours.
“Our primary focus is 911. We can’t take that truck out of the county,” said DeLorenzo, who serves as a paramedic on one of the ambulances when he is on the clock. “There’s really nothing we can do.”

While hospitals across Indiana handle many types of injuries just fine each day, severe injuries require greater attention from doctors and staff at a trauma center.
In trauma care, time is everything. Minutes matter.
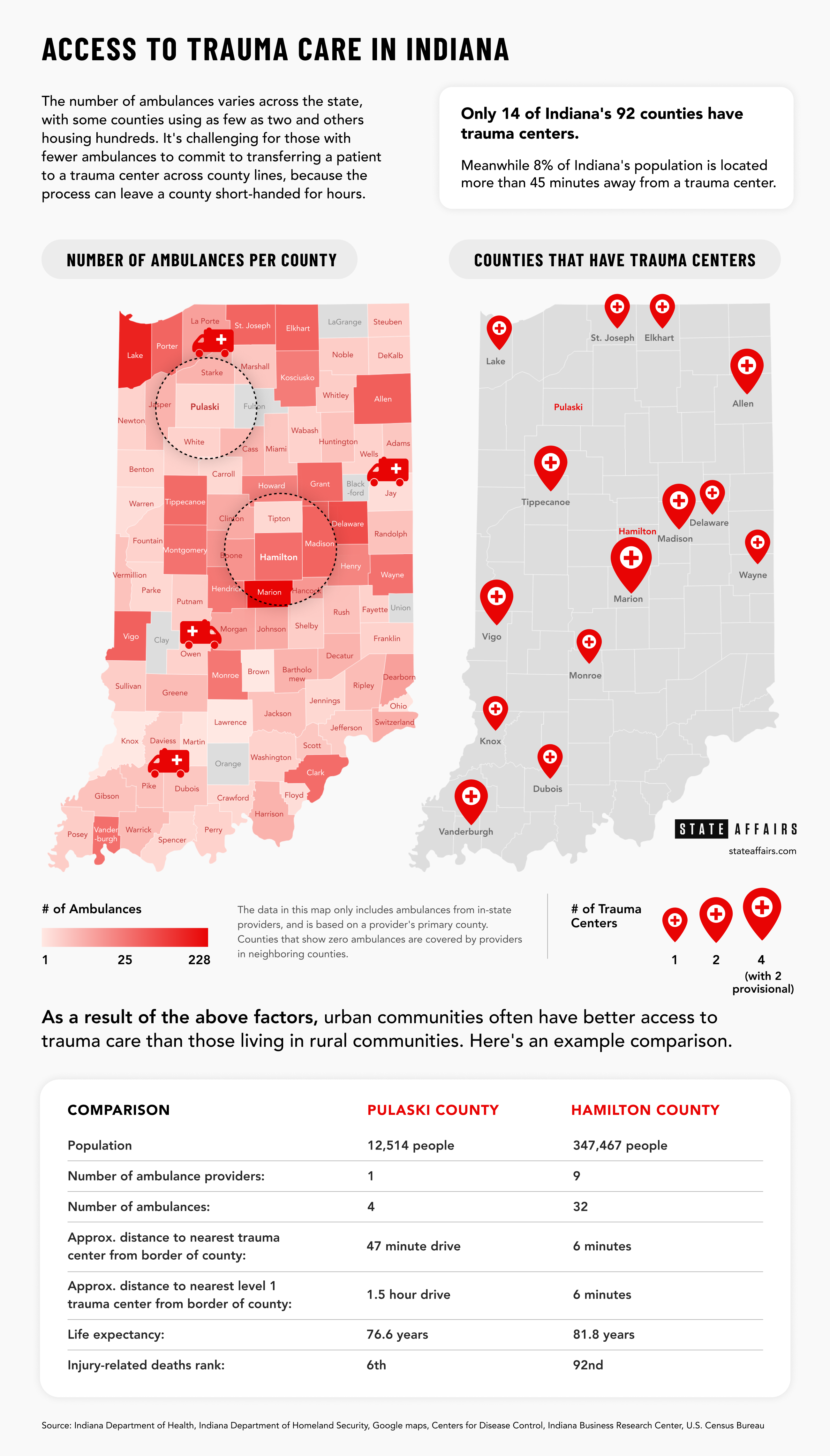
The problem? Indiana’s 24 trauma centers are primarily clumped around big cities while nearly 1 in 10 Hoosiers live more than 45 minutes away from one.
Complicating matters further, rural communities like 12,500-person Pulaski County struggle to obtain the equipment and hire the people necessary to run ambulances that they’ve already bought.
That can have consequences. Greater shares of Hoosiers are dying because of injuries compared to the U.S. average, according to Centers for Disease Control age-adjusted data from 2016-2020. That signals a trauma care problem in a state that already struggles with low life expectancy. The leading causes of death for Hoosiers aged 1 year to 44 are preventable injuries.
Anyone can experience a traumatic injury, but the problem can be exacerbated in Indiana’s less-populated areas, where a higher percentage of crashes are fatal. Pulaski County, for example, had the highest rate of fatal automobile collisions per person in 2020, and similarly high injury fatality rates over the past five years.
“We just need to fill in the gaps, so that it doesn’t matter whether you live in Indianapolis or Bath, Indiana,” said Dr. David Welsh, a general surgeon in rural southeast Indiana who is on the Indiana State Trauma Care Committee. “You deserve to get good treatment, and good treatment in trauma care makes a difference.”
Unlike other states, Indiana does not possess a statewide trauma plan to coordinate trauma centers, community hospitals and EMS providers. Nor does the state consistently fund trauma care. In a recently released report, the American College of Surgeons (ACS) criticized the system as “generally fragmented and not well coordinated.”
The problems have grown so urgent that they’ve drawn the attention of Gov. Eric Holcomb and leading lawmakers. His administration is attempting to revamp the system and is seeking more money for the state’s trauma system, but it’s not yet clear if it amounts to a Band-Aid when the system needs open heart surgery.
The disparity is evident
One thing Holcomb’s administration wants to do is reduce the number of Hoosiers who live more than 45 minutes away from a trauma center.
That’s because receiving care at a trauma center lowers an injured patient’s risk of death by 25%, according to a 2006 study.
“If you get to a trauma center within the first hour after your injury, then your risk of death or significant comorbidity is significantly reduced,” said Dr. Lindsay Weaver, an emergency medicine physician who serves as Indiana’s chief medical officer.
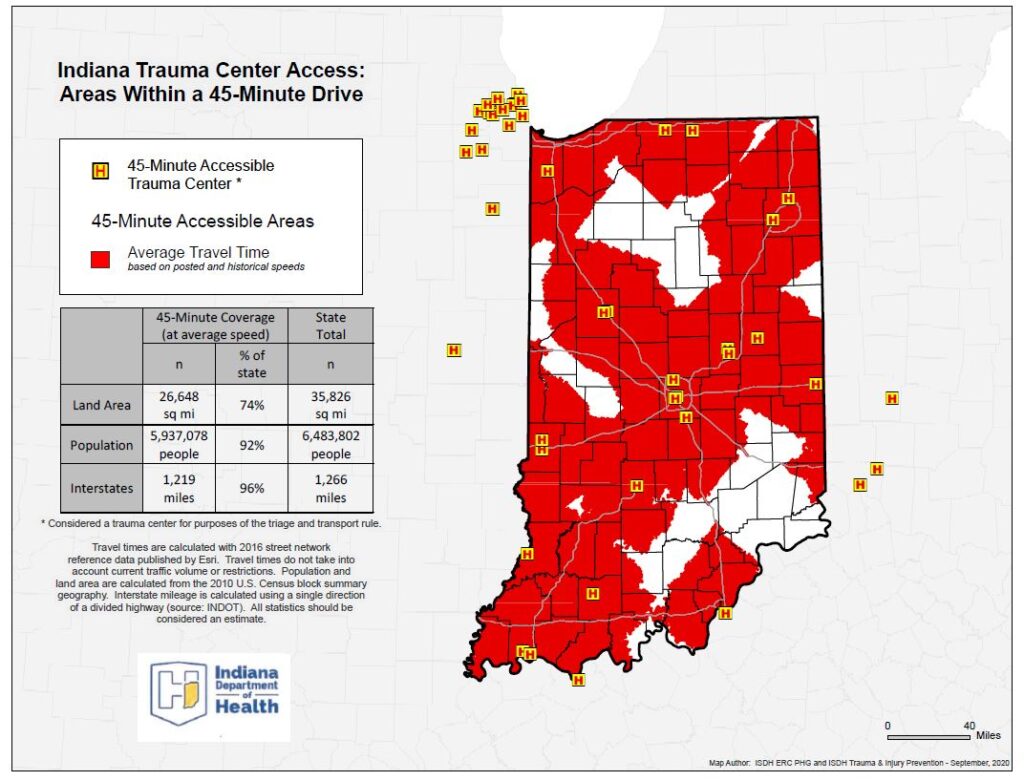
(Credit: Provided by the Indiana Department of Health)
In Indiana, the age-adjusted injury mortality rate is significantly higher in those regions of the state with no trauma centers, according to the ACS report.
That disparity is evident in the state’s motor vehicle fatality statistics.
Marion County, home to the most trauma centers, had by far the highest total number of collisions in 2020, but it ranked in the bottom half of counties in terms of the percent of crashes that were fatal.
Switzerland County, which is more than 45 minutes away from a trauma center and has no hospital, consistently has a higher percentage of collisions that are fatal than other counties.
“An effective trauma system saves lives, reduces irreversible disabilities and increases quality of life,” said Dr. Paul Halverson, dean of the Indiana University Richard M. Fairbanks School of Public Health. “If you can help save the lives of a young person or reduce their disability but keep them working and productive, it’s not only a good thing for the individual, but it’s a wise investment because they go on to be a productive part of society.”
Helicopters are able to dramatically cut transport times, but they’re usually reserved for the most extreme injuries and can’t fly when the weather is bad.
The number of trauma centers in Indiana has increased substantially since 2008 when there were only seven, Weaver points out. But even today, only Marion County is home to the highest-level trauma center. It’s also the only county with a pediatric trauma center.
Meanwhile, all of Indiana’s neighbors have the highest level of trauma centers scattered in multiple counties across the state.
To start, the Indiana Department of Health is examining hospitals located in Indiana’s dead zones and hoping to transition three into trauma centers.
Closing the gap
Becoming a trauma center, though, would be a tall order for many rural hospitals.
For one, hospitals would have to increase staffing. Even at a Level III trauma center, such as the ones in Elkhart or Bloomington, an orthopedic surgeon must be on site 24 hours a day, and patients must have access to anesthesia and radiology services within 30 minutes. Trauma centers also are required to have a designated injury prevention professional.
Rural hospitals can struggle to keep their doors open and recruit physicians. A report from the Center for Healthcare Quality and Payment Reform found that six unnamed rural hospitals in Indiana are at immediate risk of closing. Further complicating the matter, Indiana lawmakers are pursuing multiple bills intended to lower the cost of health care. Hospitals warn that could have unintended consequences: the closure of hospitals.
Already, more than a dozen rural counties don’t have a single hospital.
Other states provide grants to encourage hospitals to transition to trauma centers, but not Indiana. Arkansas, for example, even provided incentives to hospitals in neighboring states that were closer to many Arkansas residents, said Halverson, the IU dean.
He previously worked as director of the Arkansas Department of Health, where he helped establish the state’s trauma and centralized dispatch systems.
But even if the state provided more funding, multiple rural emergency room leaders told State Affairs it doesn’t make sense for them to transition to a trauma center.
They don’t see the volume of patients necessary to justify buying new equipment or hiring specialized doctors, such as trauma surgeons or neurologists. On top of that, doctors need patients to remain updated on their skills and training.
“To be an expert, you’ve got to do something at least 10,000 times,” said Dr. Ted Seall, Pulaski Memorial Hospital’s emergency department medical director. “For us to get 10,000 gunshot wounds here in Winamac, that would take forever.”

Right now, his emergency room sees about 15 patients a day.
In addition, smaller hospitals typically do not stock the large volumes of blood needed for some trauma patients.
Some states, such as Arkansas, have created a fourth trauma center tier in an effort to bring more hospitals into the system without expecting them to have the same resources as big-city hospitals. But Indiana doesn’t have that option for hospitals.
It’s not that Indiana needs a bunch of Level I hospitals; Indiana needs a functioning and coordinated system, Halverson said.
Lack of EMS providers
If Indiana state government wants to help by creating new trauma centers, rural communities have another idea: Help the EMS.
Hospital administrators say they regularly struggle to transport someone, whether it’s because they can’t find a hospital to admit the patient or there simply isn’t an ambulance available. Hospitals are required to admit patients that arrive directly from a scene. That’s not the case for those coming from another hospital. The delays can last 12 hours or more.
It’s a problem across the state. From 2019 until the third quarter of 2022, at least 29% of trauma patient transfers were delayed, with the most common known reason for delay being an EMS issue.
In Madison, driving to Louisville takes about an hour each way. Occasionally the local hospital’s EMS needs to drive further for certain specialized care, such as behavioral health. When the ambulances are on the road and unavailable, it creates a backup in the Norton King’s Daughters’ Health emergency room while patients wait for their turns to be transferred.
“Transfers are a big part of what we do because we’re all rural,” said Carol Dozier, the CEO of the hospital. “Sometimes we have to go a pretty long distance to get someone to the right facilities.”
Roughly half of Indiana counties have only one ambulance provider, according to Indiana Department of Homeland Security data, and 16 counties reported having as few as four ambulances or less. A handful of counties rely entirely on EMS providers in neighboring counties.
And those numbers appear rosier than reality. Not all of the ambulances are in use due to a lack of staffing. Similarly, some ambulance crews are able to treat only basic injuries.
A staffing shortage, caused in part by low wages, is driving the disparities in care. Rural EMS providers are competing with other health care industries that simply pay better, as well as providers in larger cities, to attract talent.
EMS providers say they struggle to afford the costs associated with training paramedics, let alone attracting enough people into the field in the first place.
The Medicare reimbursement rate isn’t enough to cover the cost to transport patients, and there is no separate funding from the state to run these programs. That means it often falls to local governments or hospitals to eat the costs associated with running EMS.
And the cost of new ambulances is skyrocketing. In a typical year, the cost of a new truck grows about 5% every year; last year, though, it jumped by 35%, said Dr. Scott Smith, a longtime emergency room doctor who runs Adams Memorial Hospital in Decatur.
“Our EMS operates at a loss,” Smith told State Affairs, “and has for as long as I can remember.”
That leaves little left over for salaries and training in some communities with small populations and budgets.
(Credit: Brittney Phan for State Affairs)
In Harrison County, a 40,000-person county near Louisville, the hospital EMS was so understaffed until recently that it operated with three trucks, instead of the usual five, said Jeremy McKim, the EMS manager.
But the situation is worse in neighboring Crawford County, which does not have a hospital and at times runs only one ambulance. Sometimes Harrison County EMS has to chip in, McKim said.
“We’ve got to figure something out to get people into our industry,” McKim said. “The staff is aging and they’re not going to continue to do this. The rate of people coming into this industry is not meeting the numbers of people leaving.”
Indiana lost 233 ambulances and 1,075 EMS clinicians between 2018 and 2021, according to the ACS. The staffing problems have been exacerbated by a 66% increase in ambulance runs from 2018-2021, said Kraig Kinney, Indiana EMS state director, during a State Trauma Care Committee meeting last year.
“It’s a nationwide trend,” Kinney told State Affairs. “That’s part of the reason the workforce shortage is showing up right now, because not only are we tighter on number of people available, but we have more needs, so everyone is busy.”
How Indiana hopes to fix the problem
State health leaders realize the trauma system has gaps. In fact, it was the state that invited the ACS to evaluate Indiana’s system in November.
But the list of recommendations from the ACS is lengthy, and ranges from creating a trauma system performance improvement plan, to completing an EMS workforce assessment, to securing ongoing funding. The ACS, though, did not recommend a specific dollar amount needed to rightsize the system.
The two-year proposed budget contains $9 million over two years for “trauma system quality improvement,” which Weaver said can be used to better coordinate trauma care across the system, identify current problems using data analysis and focus on prevention. Ultimately, the Trauma Care Commission — which would be codified under the public health bill, Senate Bill 4 — would provide oversight on how to best use that money, she said.
Is the money enough? “I think you have to start somewhere,” Weaver told State Affairs.
There’s no guarantee that funding will go toward encouraging more hospitals to become trauma centers or current trauma centers, despite the recent recommendation from the ACS to provide financial incentives encouraging participation in the state trauma system in both its 2008 and recent report.
An additional $14.6 million would be set aside for EMS under the budget that can be used for recruitment, training and new ambulances. It also can be used to ensure the closest emergency departments are responding when dispatched.
The state is also already undergoing the recommended EMS workforce assessment. Plus, if SB 4 passes as is, the Trauma Care Commission would be tasked with developing a statewide trauma plan. Some changes might also have to come in future years.
The House passed the budget Thursday and the bill now moves to the Senate, where Senate President Pro Tempore Rodric Bray, R-Martinsville, and other senators have signaled a willingness to fund the trauma care proposal.
"We live in a state where a significant impact on how long you live, is where you live,” Sen. Ed Charbonneau, R-Valparaiso, said when discussing SB 4 on Thursday.
But perhaps nothing shows the need for trauma care system changes more than an anecdote DeLorenzo shared of a patient who fell off the roof of his home. Because of the winter weather, no emergency helicopter could fly, which meant the man had to be transported to the local, non-trauma center hospital to be stabilized.
After he arrived at the local hospital, though, staff struggled to find a trauma center that could accept the patient, he said. The only option: a Level III center, when in reality, DeLorenzo said the man’s injury would usually need a higher caliber trauma center.
On top of that, icy roads slowed the drive to two hours.
“That was not good for that patient,” DeLorenzo said. “We’re in the middle of nowhere, so when you’re max speed of 30 miles per hour, trying to stay on the road and go 20 miles to a call, it takes a long time.”
While DeLorenzo is not certain whether the patient survived his injuries, he still wonders if he had been transported more quickly, or had been moved to a higher level trauma center, whether the man’s chances of survival would be greater.
Contact Kaitlin Lange on Twitter @kaitlin_lange or email her at [email protected].
Contact Ryan Martin on Twitter, Facebook, Instagram, LinkedIn, or at [email protected].
Twitter @StateAffairsIn
Facebook @stateaffairsin
Instagram @stateaffairsin
LinkedIn @stateaffairs
Header image: Pulaski County EMS, which typically runs two ambulances across the county's 435 square miles of mostly farmland, is headquartered in Winamac, Indiana, Feb. 7, 2023. (Credit: Ryan Martin)
Read this story for free.
Create AccountRead this story for free
By submitting your information, you agree to the Terms of Service and acknowledge our Privacy Policy.
Holcomb says he’s confident of investments from Brazil, Mexico trip
Gov. Eric Holcomb wrapped up his weeklong travels to Brazil and Mexico by saying he expected new business investments to emerge from the trip. Holcomb told reporters Thursday night from Mexico City that he had many productive meetings with government and business leaders promoting Indiana’s agriculture ventures. “It really does remind me that face to …
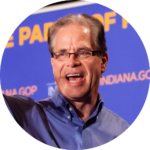
Mike Braun on why he wants to be in politics ‘at a level of significance’
EDITOR’S NOTE: This is one in a series of profiles of the candidates running for Indiana governor.
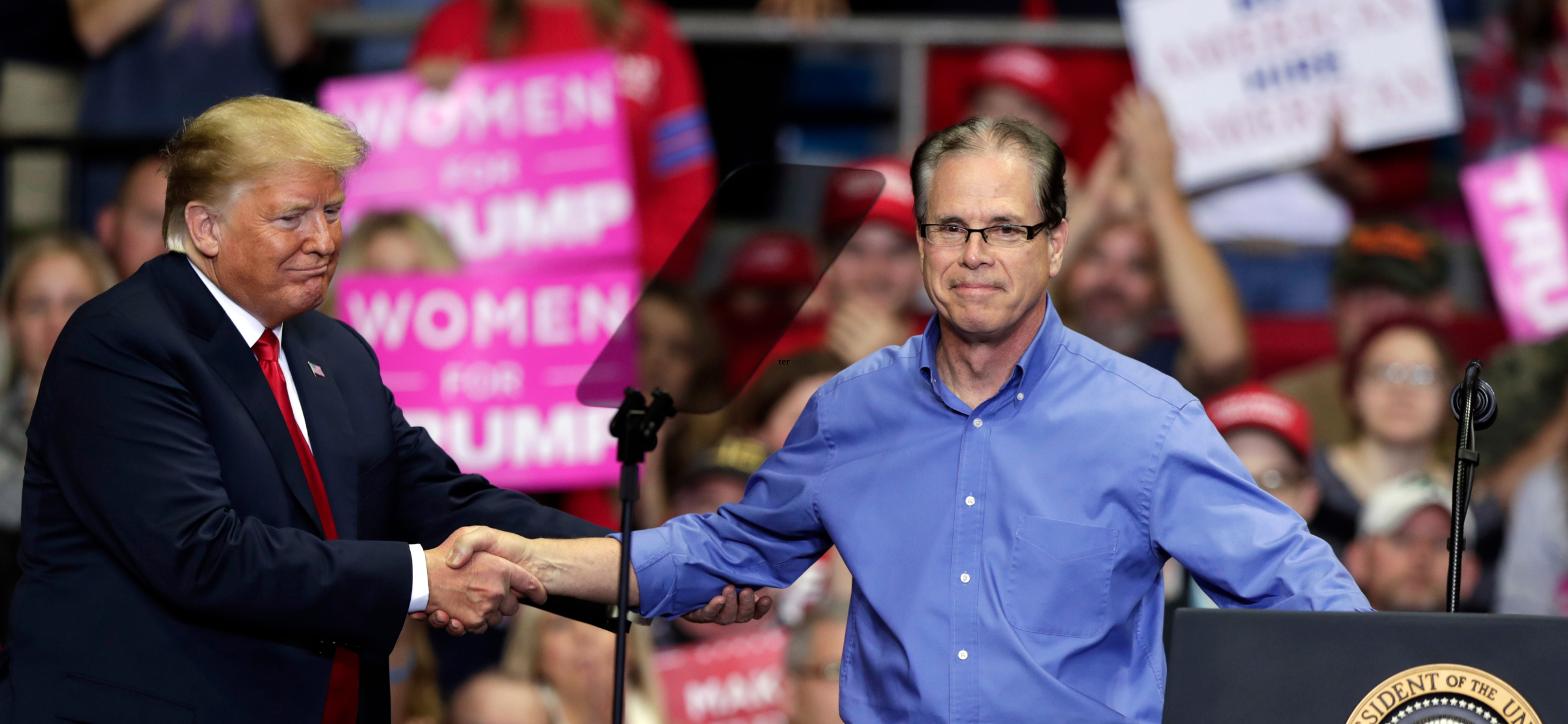
JASPER, Ind. — Mike Braun was a former two-term state representative in 2018 when he compared himself to the ultimate “outsider”: President Donald J. Trump.
Braun used that label to defeat two sitting congressmen in a Republican U.S. Senate primary race he had begun with about 1% of support in an internal poll. Then he used five Trump Make America Great Again rallies and $11 million of his own money (and another $20 million from an undisclosed donor) to upset Democratic U.S. Sen. Joe Donnelly.
“Here, we come in as a sitting senator — it’s a much different dynamic in how the political market is going to accept you,” Braun said of his current campaign, as opposed to the one he largely self-funded in 2018. (A conciliation agreement made public in late March revealed that the Federal Election Commission fined Braun’s 2018 campaign $159,000 for failing to properly disclose more than $11 million in transactions from July 2017 through December 2018.)
“I think we’re in good shape because we’re fairly solid when you look at the record I’ve got,” he said of the current campaign, in which he repeatedly invites Hoosier voters to examine his record in office. “Politically, this is less of a mystery in terms of what to do. We just need to execute in a similar way to what we did in ’18 and get the message out that will resonate with Hoosiers. I feel confident we’re going to be able to do that.”
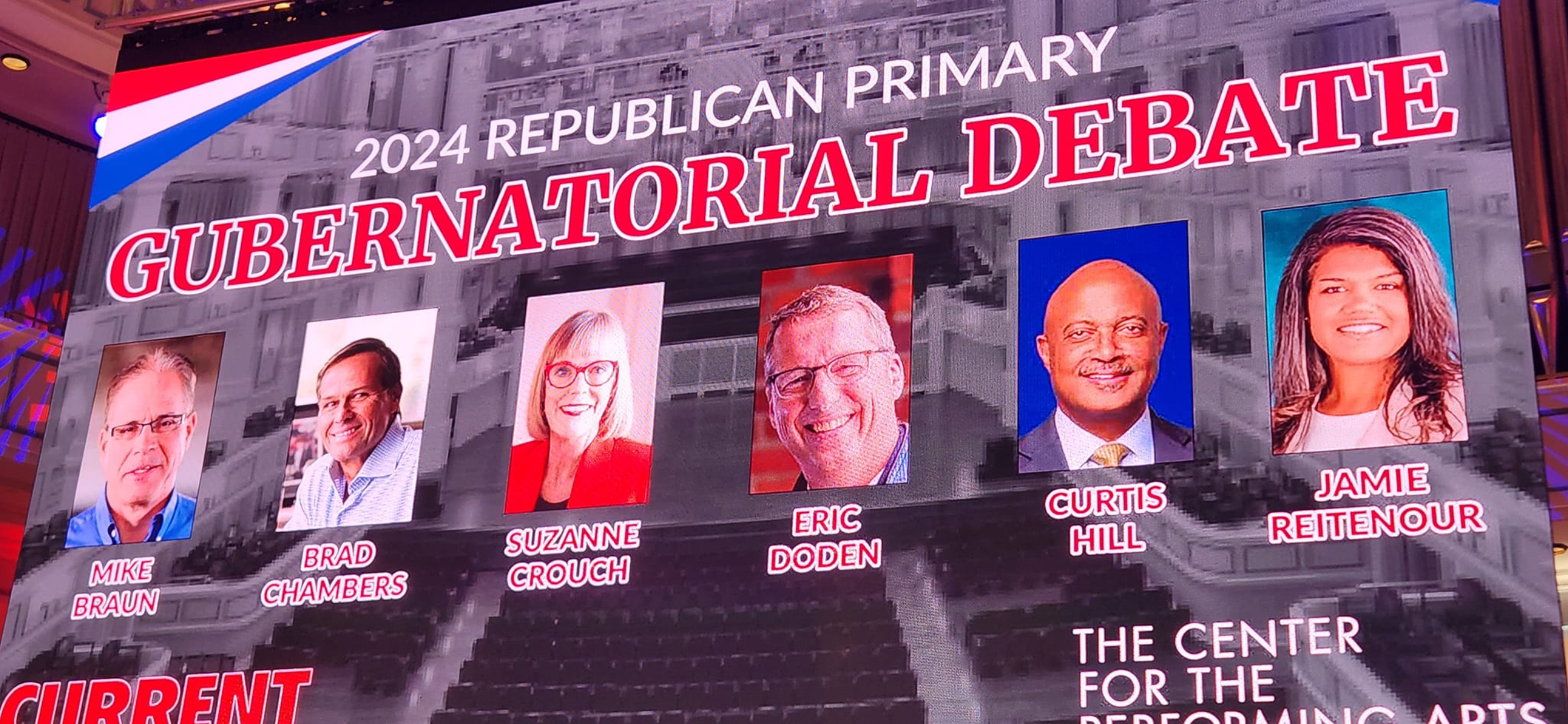
Sen. Braun continues to bill himself as the “outsider” — along with former Commerce Secretary Brad Chambers — as he steers through an unprecedented six-person Republican gubernatorial field that also includes Lt. Gov. Suzanne Crouch, businessman Eric Doden, former state Attorney General Curtis Hill and Indianapolis mom Jamie Reitenour.
Normally, Hoosier Republicans coalesce around a single candidate for an open governor’s race, often turning a simple candidacy into a movement. But not this time.
Past Republican nominees and governors were not outsiders — they were ultimate insiders. Edgar Whitcomb sought the office while serving as secretary of state; Doc Bowen as speaker of the House; Richard O. Ristine, Robert Orr and John Mutz as lieutenant governors; Linley Pearson as attorney general; David McIntosh and Mike Pence as congressmen; Mitch Daniels as an outgoing White House budget director; and Eric Holcomb as a former aide to Daniels, U.S. Rep. John Hostettler and U.S. Sen. Dan Coats (before becoming a state GOP chair and then lieutenant governor).
Toward the end of the first homestretch debate at the Carmel Palladium on March 11, Hill wondered why Braun was seeking the governor’s office if his one term in the U.S. Senate had been so successful.
“I thought he was very well equipped for the job,” Hill said. “He talks about how tough it is in D.C. I want him to go back and continue the fight; he gave up the fight. Will he give up the fight as governor?”
Braun responded, “I spent 37 years building a little scrappy business into a regional, national and international company. And that is what I ran for Senate on. It resonated overwhelmingly. If you like me as your senator, you’ll like me better as governor.”
Throughout Indiana history, former governors — from Oliver P. Morton to Evan Bayh — found career-end refuge in the U.S. Senate. Braun is doing it in reverse.
“You know why?” he asked in his unassuming office at his company Meyer Distributing in Jasper. “Because they’re from the farm system of politics. The people who got done being governor just weren’t done with politics. They wanted to continue. My blessing is I did something in the real world first before I decided to get into politics at a level of significance.”
Asked if he is more of an executive than a legislator, Braun responded, “I feel I’m good at both because legislatively I knew what to get done as a legislator. I passed a unique regional authority bill that helped us down here on a road project we talked about for 40 years in the abstract. To me, if you’re an entrepreneur, you know how to get from here to there.”
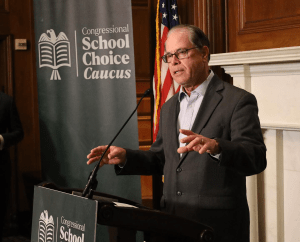
During the Carmel debate, Braun called himself the “most fiscally conservative” Republican and a freshman who has been honored by independent groups for passing legislation. Chambers reminded him: “You’ve been in the Senate for an additional $7 trillion to $9 trillion in borrowing.”
Asked if he would like to make a rebuttal, Braun said, “I think I’ve got one,” while the audience laughed.
Braun is proud of his Senate record. “I base that mostly upon all the hard work invested as a senator, but a record that is generally resonating with Hoosiers and the fact that I visit all 92 counties each year,” he said. “Something you probably aren’t aware of, but we recently announced we’ve completed 11,000 cases for Hoosiers. We did that on behalf of veterans, immigration, Social Security and the whole spectrum of how you can get entangled with the federal government. That is one of the proudest parts of being a U.S. senator.
“It’s very important for anyone who wants to lead our state [that they’d] better be there with a track record,” he said at the Carmel debate. “You won’t have to figure out what they might do when they say they want to aspire to something like this. You need to be willing to flesh out those ideas. Of anyone on the stage here, I have the most recent track record on what’s happened, when you have to vote, what you’re really for, not what you say you’re going to be for.”
“I think when [Braun] talks about being a proven conservative, he’s served in the U.S. Senate for six years and has votes that can reaffirm that,” Laura Merrifield Wilson, an associate professor in the History & Political Science department at the University of Indianapolis, told State Affairs. “He had been in the General Assembly before that and could point to certain things. That’s going to help especially with your Republican primary in the state of Indiana, which is going to be very heavily conservative.”
Braun and the city of Jasper
To understand what makes Mike Braun tick, you have to travel to Jasper, a small city about an hour northeast of Evansville. “I have been blessed to be raised in a place like Jasper,” he said during the Carmel debate. “It’s a community based on faith, family, freedom and opportunity.”
Braun left Jasper to attend Wabash College and then earned a Master of Business Administration from Harvard University. He said many of his classmates went to Wall Street or Silicon Valley, but he headed back home. He bought what he calls a “hardscrabble” company — Meyer Body — and built it into a sprawling 1,500-employee national enterprise that distributes various products, from auto parts to industrial supplies.

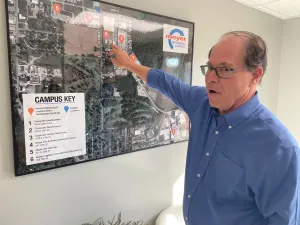
“There’s no substitute about seeing the context of where you’re coming from,” the 70-year-old said last November during a walking tour of this 270,000-square-foot complex. “My major piece of work — you’re looking at it right here.”
In Hoosier politics, a candidate for governor most likely points to his public service record, which in Braun’s case is his 10 years on the local school board, three years in the Indiana House and five-plus years in the U.S. Senate. But he attributes much of his policy underpinnings to the seven acres in Jasper that are home to Meyer Distributing. It is a beehive of activity, with beeping forklifts and transporters shifting and loading product onto tractor-trailers while Aerosmith rock music blares in the background.
It was here 15 years ago where he pursued a new path toward providing more cost-effective health care options for his employees that has transformed his viewpoint on commodity-draining states and private industries. “I fixed health care in my own business, have healthier employees, cut costs 15 years ago, created health care consumers out of my employees and know some of the things I can do for coverage of our own state employees,” he said.
“We’ve got one of the highest health care costs of any state and some of the poorest health care outcomes,” Braun added.
Will that translate to 6.8 million Hoosiers? Can you take those fundamental building blocks on health coverage and bring them to the masses?
“Sure, you can,” he responded. “That’s owning your own health care and well-being. That’s basically what I did here. I gave the best tools to my employees to do that. I put skin in the game on their minor health care to where they shop around for the small stuff, and they’ve got the best coverage when they get critically ill or have a bad accident. Insurance companies told me all of that. They were making so much money on our plan back then I decided to self-insure and basically solved health care as most companies would love to do, but had to be entrepreneurial. I just basically took what the insurance companies told me, saw how much money they were making covering my business, created it as a cost center and not a profit center and that’s how I fixed things.”
What would a Gov. Mike Braun administration look like?
“What I’ll bring to bear as the governor will be someone who will be entrepreneurial politically,” Braun said. “To me, if you’re a good entrepreneur, politics is easier than building a business. It’s just got tighter compression in terms of the political hurdles you need to jump.”
On his campaign website, Braun expresses optimism about Indiana’s future and says his concerns for the next generation’s welfare are driving his run for governor. Having served Hoosiers in Washington, he believes that solutions to the state’s issues lie locally, not with “special interests and career politicians in D.C.”
Braun has laid out a 12-point agenda that includes growing Hoosier jobs and the economy; improving education; implementing affordable health care; embracing reliable, affordable and clean energy; preserving agriculture; and cutting taxes while reducing the size of government.
His campaign website also addresses hot-button issues:
- “Put kids first” by “making sure divisive theories like critical race theory or discussions about sexual orientation and gender identity have no place in our public schools.”
- “Protect parental rights”: He will fight to “protect the rights of parents to shield their children from divisive ideologies by ensuring parents have transparent access and meaningful input on curriculum and materials in our schools.”
- “Stand up to woke corporations”: He says, “ESG [environmental, social and governance] puts investors and retirees at financial risk and will have no place in the Indiana state government.”
- “Pro-life means pro-family”: “State lawmakers must work to ensure the gains we have made to protect life are secured and strengthened, while working to help mothers and their infants receive the care and social support they deserve to ensure a healthy start to life.”
- “Standing with law enforcement”: He vows “to make sure the justice system is not failing them [law enforcement] by refusing to detain dangerous criminals, manipulating the bail system, and intentionally refusing to enforce laws based on a political ideology.”
- “Securing our southern border”: Braun explains, “Joe Biden and the left have created a humanitarian and national security crisis on our southern border. [I] will work to fund solutions that keep criminals and drugs, like fentanyl, from entering our country.”
- “Defend our constitutional rights”: “The rights of law-abiding gun owners, the freedom to practice our religion, and the rights of parents to protect their children from leftist ideology are under attack.” He says he “will never waver when it comes to defending every Hoosier’s rights to life, liberty, and the pursuit of happiness.”
- “Election security and reform”: “The right of Americans to cast their vote in fair and secure elections is essential to the survival of our Republic. Hoosiers must trust that our elections are free from fraud and guarantee that every legal vote is counted accurately.”
- “No more mandates or lockdowns”: “The lockdowns during the COVID-19 pandemic were a disaster for our state and led to business closures, job losses, mental health issues, learning loss, and still failed to protect the most vulnerable. As Governor, Mike Braun will never lockdown our state, mandate masks for our kids, or tell someone their job or business is not essential.”
At the Palladium on March 11, Braun added that the government “came up with the term ‘you’re essential; you’re not essential’” during the COVID-19 pandemic. “I never thought that would happen in our own Hoosier State,” he said. “When you have that type of bureaucratic determination, try to explain that to my wife and all the other merchants in downtown Jasper. They were out of business for a long time. You never know when it’s going to creep into your own state. It was very disappointing.”
Endorsed by Trump
Braun possesses one important element in his primary race: the imprimatur of Donald Trump. “I can tell you that every one of my opponents would have loved to have the endorsement in a state like Indiana,” he said in his Jasper office.
When Trump endorsed Braun, the former president was facing 91 criminal charges in two federal jurisdictions and two in Manhattan and Georgia (since reduced to 88 when three charges were dropped in Atlanta).

“There’s a political intertwining,” Braun said of the charges facing Trump, who the senator has twice voted to acquit during Senate impeachment trials. Following his 2021 acquittal vote, Braun said, “The riot on January 6th was horrific and should be universally condemned, and while I listened to both President Trump’s defense and the House Managers’ arguments, I believe it is unconstitutional to hold a trial to remove a former President from an office he no longer holds and feel a vote to convict would have deep negative implications for the First Amendment and due process.”
“Whether those indictments get parlayed into a conviction, I’m just extrapolating what I see Republican primary voters are doing,” he said. “I don’t think that makes much difference.”
In the days leading up to Jan. 6, 2021, Sen. Braun was supportive of efforts to challenge Electoral College certification. But after the Trump-inspired mob overran the U.S. Capitol, assaulting more than 150 cops while seeking to hunt down Vice President Mike Pence, Braun reversed course, saying he “didn’t feel comfortable with today’s events.” He said election integrity is “still a valid issue.”
Since Jan. 6, Trump has talked about nullifying the U.S. Constitution and called for the execution of the outgoing chairman of the Joint Chiefs of Staff, Gen. Mark Milley. Does that type of rhetoric concern Braun?
“Obviously, that stuff is not the stuff I would put out there,” he responded during the November tour of his company. “I think that hurts rather than helps the cause because it further polarizes the people that might even like his policies. That’s a difference in approach. I respect everyone’s ability on how they’re going to sell themselves. I would stick on looking at the record in terms of the way it was pre-COVID, and the stuff you can’t change, I don’t know really what the point would be to further talk about it, because you can’t fix it. That toothpaste is out of the tube.”
Wilson of the University of Indianapolis said of Braun: “He’s been able to effectively align himself with Donald Trump. He did that back in 2018, in the Republican primary for U.S. Senate against Todd Rokita and Luke Messer. He was clearly the Trump candidate, and that plays well in Indiana, where Donald Trump has won by 20% in the last few presidential election cycles.”
What type of governor would Braun be?
When Mike Braun served on the local school board, Mitch Daniels was governor. During Braun’s three-year General Assembly tenure, Mike Pence and Eric Holcomb were governors. What did he glean from their leadership styles?
“I’ll be able to distill best practices,” he said. “Look what Mitch Daniels did. He came in 2004, he inherited a budget that was in the red that had been run recently by Democrats. So he had to get the state’s financial cash flowing. And then you look at what he did when he started to address issues. We are the ‘Crossroads of America’ and we weren’t even funding roads the right way. Almost every penny of the fuel tax was being spent on other stuff. He started fixing things that would have been most apparent that needed to be fixed.”
Braun noted that Gov. Daniels wasn’t afraid to spend political capital.
“One reason he did that with good leadership, besides the fact that he’s a brilliant mind, was he was also willing to take risks,” Braun said. “If you’re not willing to take risks, you’re going to be in a broad band of mediocracy, whether it’s in business or government. You don’t want to take on too much; you want to leave your neck intact politically and operationally, and he was willing to do that. I think Pence and Holcomb inherited a much better-run state government and have enhanced it in their own ways since then.
“The difference between me and a Pence or a Holcomb would be [that] I spent my time in the trenches of building a business from scratch,” added Braun, who said he will continue to invite anyone to Jasper on Fridays to talk about issues. “That’s why I took time to show you.”
Statehouse reporter Rory Appleton contributed to this story.
about Braun
- Age: 70
- Hometown: Jasper, Indiana
- Education: Master of Business Administration, Harvard Business School (1978); Wabash College (1976)
- Family: Married to Maureen Braun since 1976, with four children, Ashley, Kristen, Jason and Jeff
- Job: U.S senator from Indiana since 2019
- Work history: Member of the Indiana House of Representatives from the 63rd district from 2014 to 2017; owner of Meyer Distributing (formerly Meyer Body) since the mid-1980s
read these related stories
- Eric Doden is running from behind but hopes his ‘bold vision’ will propel him forward
- Suzanne Crouch positions herself as a ‘different’ candidate for the voiceless
- Who is Jamie Reitenour? Indianapolis mom mobilized volunteers to make governor’s ballot
Brian Howey is senior writer and columnist for Howey Politics Indiana/State Affairs. Find Howey on Facebook and X @hwypol.
Who is Jamie Reitenour? Indianapolis mom mobilized volunteers to make governor’s ballot
EDITOR’S NOTE: This is one in a series of profiles of the candidates running for Indiana governor.
ZIONSVILLE, Ind. — It wasn’t the largest campaign event the 2024 election cycle is likely to see.
About 15 people, some of them children, gathered on a rainy April night at Our Place Coffee, nestled just feet from the watchful eye of Zionsville’s Abraham Lincoln mural. But Republican gubernatorial candidate Jamie Reitenour, an Indianapolis mom with no previous political experience, spoke with every single one of them.
It was one part coffee-and-issues politicking and one part informal Bible study, complete with scripture quiz questions for the kids in attendance.
Reitenour, well-worn Bible in hand, shared her oft-repeated story of being called by God to run for governor about six years ago — a destiny confirmed by friends and strangers alike along the way, she said. This charge, she told the group, would allow her to rise above traditional campaign currency, such as fundraising dollars and polling numbers.
Suzanne and Shon Hough sponsored the event after meeting Reitenour at their shared church, Horizon Christian Fellowship in Lawrence.
“As soon as we met her, we knew this is someone to support,” Suzanne Hough said. “We knew she wasn’t a politician. She was called. She has a love and compassion for people.”
That is how Reitenour has made it this far — how she gathered the 4,500 state-mandated signatures to qualify for the May 7 primary ballot, how she’s made it onto a stage filled with more experienced and wealthier opponents. For more than a year, she’s hosted several small events per week throughout the state, traveling some 35,000 miles, by her count.
The dozen or so latte-sipping supporters had a part to play, the candidate said.
“Go to your contact lists and tell them about our Facebook,” Reitenour said. “We could reach 144 people today if we all did that.”
The call
Reitenour’s purpose changed in 2017 while walking through downtown Indianapolis with her husband, Nathan.
“I just heard a whisper: You’re going to be the governor of Indiana,” Reitenour told State Affairs.
The couple wandered over to the governor’s mansion.
“We looked at it and thought, ‘That does not look like our family,’” she recalled. “So I just put the calling on the shelf.”
Indiana requires gubernatorial candidates to have lived in the state for at least five years. She had only just moved from Michigan.
Reitenour believed the country was in a good spot under then-President Donald Trump. Why would she need to run?
“I just thought about it,” Reitenour said. “Why would the Lord call an ordinary person to something like that when the nation was doing so well? But the reality of scripture is that you see these times where people are called, and you can see the reasons for the calling around them.”
Her regular Bible contemplation soon took her to the Book of Nehemiah, who was a governor. Another sign, she said.
The state’s response to the COVID-19 pandemic set off alarm bells for Reitenour, who considered steps like mask requirements an affront to personal liberty. She brings up the subject often, and it made it into her coffeehouse remarks.
“How am I in a conservative state, but I don’t feel free?” she told the crowd.

After COVID-19 and the election of President Joe Biden, Reitenour began to think more seriously about running for governor.
Her mission was affirmed first by a close friend, whom Reitenour said received a similar calling from God to help her candidacy, and then by strangers, whom she said confirmed her destiny during separate chance meetings at a Panera Bread location.
She began to meet with church groups and advocacy organizations that align with her views, including Moms for Liberty and Indiana Right to Life. Despite being referred to as an activist on the campaign trail, Reitenour said she is not part of any activism group.
Getting on the ballot
This network of like-minded supporters would soon serve as the volunteer arm of Reitenour’s campaign.
Indiana requires candidates for governor to collect at least 4,500 signatures from voters, including at least 500 from each of the state’s nine congressional districts. It’s a tall order even for seasoned politicians, who often hire specialized operatives for the task.
“The mystery of how we did that will also be the mystery of how we win,” Reitenour said.
She focused on growing supporters and gathering signatures at each small event she hosted, then mobilizing those attendees to gather still more for her.
“I had a formula in my heart for this that the Lord gave me at 4 a.m. one morning,” she said.
The campaign
Reitenour made the ballot, but she is the least-known candidate in a field that includes Sen. Mike Braun, Lt. Gov. Suzanne Crouch, former state Attorney General Curtis Hill, former state Secretary of Commerce Brad Chambers and Eric Doden, a Fort Wayne businessman and previous president of the Indiana Economic Development Corp.
She has no previous political experience. She is a stay-at-home mom who also homeschools her five children and volunteers through ministry. Her previous work experience includes compliance management at a mortgage company, secretarial work and even a stint as an assistant coach in women’s field hockey.
Reitenour was selected in the governor’s race by just 2% of respondents in a recent State Affairs/Howey Politics Indiana poll, tying her with Hill for last place behind front-runner Braun (44%). She has consistently polled in the low single digits.
While other gubernatorial candidates can draw from years of campaign fundraising experience or millions in personal finances, Reitenour had raised just a little more than $54,000 as of March 31.
She has thus found herself paddling in a proverbial ocean of campaign spending.
The four top-polling candidates — Braun, Chambers, Doden and Crouch — have spent a combined $20 million.
After participating in the first gubernatorial debate on March 11, Reitenour did not qualify for a March 27 debate hosted by WISH-TV due to her fundraising numbers, as the television station required candidates to have raised $300,000 by December.
She was also excluded from a March 26 Fox59/CBS4 debate for not reaching a 5% polling threshold. She will be included in the final April 23 debate, hosted by the Indiana Debate Commission.
Reitenour has campaigned using a constantly shuffling group of volunteers. She has only one full-time employee: campaign assistant Casey Pierce, who met Reitenour through his mother’s church.
“It just felt like the right thing to do,” Pierce said of joining the campaign. He has never worked in politics before.
Pierce called his initial meeting with Reitenour “a Holy Spirit encounter.”
Reitenour’s platform
Reitenour described education as the state’s “greatest vulnerability,” and thus her primary platform.
“The next generation is not being educated well, and this has been a long time coming,” Reitenour said.
She has received guidance from the Hamilton County chapter of Moms for Liberty, which made national headlines in 2023 after using a quote attributed to Adolf Hitler in its first newsletter. The nonprofit, which pushes against socially minded education reforms like critical race theory, subsequently apologized.
Reitenour likewise opposes ideas like social-emotional learning in classrooms. Her plan also proposes removing technology from grades K-5, calling for private businesses to sponsor classrooms and requiring all students to pursue an apprenticeship before high school graduation.
She also favors an audit of the Indiana Economic Development Corp., tax cuts, a focus on investing in small towns and generally “pointing Indiana in the direction of family.”
The future
At her coffee shop appearance, Reitenour shied away from admitting her long odds in the race.
“The political system is meant to squeeze people out, but I am working against it,” she said.
She pledged to continue organizing no matter the primary election results.

About Reitenour
- Age: 44
- Hometown: Indianapolis
- Education: Psychology degree from Missouri State University
- Family: Married to Nathan Reitenour, with five children, ages 13, 11, 10, 9 and 4
- Job: Stay-at-home mom, homeschool teacher
- Work history: Former compliance manager at Windsor Capital Mortgage, former athletic director at Calvary Christian School (at Calvary Chapel Vista church in California)
Read these related stories
- Eric Doden is running from behind but hopes his ‘bold vision’ will propel him forward
- Suzanne Crouch positions herself as a ‘different’ candidate for the voiceless
- Mike Braun on why he wants to be in politics ‘at a level of significance’
Contact Rory Appleton on X at @roryehappleton or email him at [email protected].
And subscribe to State Affairs so you do not miss an update.
Facebook @stateaffairsin
Instagram @stateaffairsin
LinkedIn @stateaffairs
Child care: Where Republican candidates for governor stand
Six candidates are seeking the Republican nomination for Indiana governor in the May 7 primary. State Affairs is providing looks at their stances on several issues. Jennifer McCormick is unopposed for the Democratic nomination.
Indiana’s high cost of child care ranks as a primary concern for many of the state’s families.
According to Child Care Aware of America, a nonprofit organization that studies child care costs, Indiana ranks as the eighth most expensive state for infant and toddler care. The cost for caring for a baby averages 14.5% of a family’s median income, while toddler care is 12.9%.
Only 5% of Indiana families can afford infant care, the Economic Policy Institute found.
State Affairs asked each of the six Republicans vying for Indiana governor — U.S. Sen. Mike Braun, former state Secretary of Commerce Brad Chambers, Lt. Gov. Suzanne Crouch, Fort Wayne businessman Eric Doden, former state Attorney General Curtis Hill and Indianapolis mother Jamie Reitenour — how they would lower Indiana families’ child care costs if elected.
Here are their responses.
Mike Braun
“The high cost of child care burdens Hoosier families and businesses, who are trying to recruit and retain the best workers. As governor, I am open to and will work on solutions that will reduce the cost of child care, which is a win for our economy and families.”

Brad Chambers
“As governor, I’ll explore strategic expansions of all-day pre-K for 3- and 4-year-olds, including potentially increasing the income eligibility level for state-funded pre-K programs. I’ll create a state-level child care tax credit that requires recipients to work to be eligible to receive it.”
Chambers said he would also explore incentives for employer-sponsored child care.

Suzanne Crouch
“First, I would lead the effort to eliminate the state’s individual income tax, which will mean more money in families’ pockets and help reduce the financial strain of child care expenses … As governor, I would propose that the General Assembly put a priority on early childhood education throughout Indiana.”
Crouch would also support the expansion of at-home and religious-based child care, she said, noting Indiana has “some of the highest relative child care costs in the country.”

Eric Doden
“I’ve offered a bold plan to expand pre-K access to every community in the state. By partnering with communities, nonprofits and education partners, we will begin addressing this important need. … We need a state with thriving communities and access to opportunity. Cost of child care concerns are downstream of family formation rates, good-paying jobs, home ownership and a host of other economic and community issues.”

Curtis Hill
“The government is not responsible for providing child care for private sector employees. Its responsibility is to dismantle the licensing and regulatory burden that prohibits new child care providers from entering the market. If we want to lower the cost of child care, we must cut the government regulations forcing child care facilities to either close or raise prices to meet unnecessary government requirements.”

Jamie Reitenour
“We cannot bear down on taxpayers for everything. We just cannot do it. But we can talk to the private sector and reason together. Can we have in-house day cares at offices? Yes. Can we have employers operate growth centers for employees’ kids? Yes. Taxpayers are not the answer; the private sector is. With competition for qualified workers, larger businesses already employ creative benefits, including child care assistance, to attract talent.”
Read these related stories:
Contact Rory Appleton on X at @roryehappleton or email him at [email protected].
And subscribe to State Affairs so you do not miss an update.
Facebook @stateaffairsin



