Stay ahead of the curve as a political insider with deep policy analysis, daily briefings and policy-shaping tools.
Request a DemoGeorgia insurance companies flout mental health parity reporting requirements

A report by the state insurance commissioner said Georgia health insurance companies offering major medical coverage did not submit sufficient 2022 information to be in compliance with state and federal mental health parity laws. (Credit: Jacob Lund)
ATLANTA — Insurance companies in Georgia that offer major medical coverage, including for mental health and addiction services, have failed to provide adequate information to the state insurance commissioner to demonstrate compliance with state and federal mental health parity requirements, according to a recent report.
A requirement of the Georgia Mental Health Parity Act of 2022, the first annual parity report by the Office of Commissioner of Insurance and Safety Fire (OCI), was released to the governor, lieutenant governor and House Speaker on August 9. The report said that of 28 responding insurers who provide major medical coverage in Georgia, none submitted enough of the parity information requested by OCI and as required by law. Another 24 insurance providers submitted no information at all.
The goal of the state and federal mental health parity laws is to ensure that insurance companies provide coverage for mental health and addiction (behavioral health) on par with physical health conditions. The information requested by the insurance commissioner’s office was designed to allow for a comparative analysis of how insurers in Georgia covered behavioral health and physical health, using data from 2022.
Of particular concern in the report was the failure by all insurers who responded to the call for data by OCI last spring to provide sufficient information related to non-quantitative treatment limitations (NQTLs). NQTLs include elements of insurance coverage such as reimbursement rates, prescription drugs, network access and tier design, pre-authorization requirements, and standards for medical providers to participate in a network.
Some insurers provided overviews of their policies and narratives that included some comparative analyses, but none provided adequate data showing how coverage was actually applied in their operations.
The insurers’ submissions were reviewed by a Data Call Review Team made up of consultants from Regulatory Insurance Advisors, LLC and OCI staff. The report said the review team recommended “targeted market conduct examinations” to review claims and appeal files for all of the noncompliant major medical insurers. Such examinations should include “submission and review of company policies, claims, procedures, internal audits and reports,” some of which were referenced but not provided by insurers.
A letter to Gov. Brian Kemp, Lt. Gov. Burt Jones and House Speak Jon Burns said the OCI will address concerns identified during such market conduct examinations “through corrective action and enforcement tools available under Georgia law.”
It is not clear from the report when further action by the insurance commissioner’s office will occur. OCI officials did not respond to a request for comment from State Affairs.
While it was provided to state leaders before an August 15 deadline, OCI has not yet posted the mental health parity report on its website. State Affairs obtained a copy from Georgians for a Healthy Future (GFHF), a nonprofit health advocacy group, which submitted a public records request for the report in late August.
Whitney Griggs, health policy analyst for GFHF, said she and other behavioral health advocates are disappointed by the spotty information provided by insurers, and are concerned about how the insurance commissioner’s office intends to hold them to account.
Griggs said she’s hopeful that OCI will perform a thorough market conduct exam on each noncompliant insurer.
“It’s a really deep look at the company’s process for approving and denying claims, setting up their networks — kind of a deep look at all of the inner workings of how they make decisions on what they’ll cover and what they won’t cover,” she said. “… And usually if [OCI] finds issues in a market conduct exam, they can fine the insurer, like they did with Blue Cross Blue Shield [which received a $5 million penalty in 2022].”
The state parity law provides for penalties ranging from $2,000 to $5,000 for each act of noncompliance by insurers in providing coverage or supplying data requested by the state. Griggs said such penalties may not be enough to incentivize adherence to the law.
“One thing that all of this is telling me is that we need to go back and revisit the language and put some more enforcement mechanisms in there for not only what happens if you appear to not be complying with parity requirements, but if you also don’t comply with the requirements to submit data,” she said.
Check out our summary on TikTok:
Related stories:
Have questions, comments or tips about Georgia’s behavioral health system? Contact Jill Jordan Sieder on Twitter @JOURNALISTAJILL or at [email protected].
Twitter @STATEAFFAIRSGA
Facebook @STATEAFFAIRSGA
Instagram @STATEAFFAIRSGA
LinkedIn @STATEAFFAIRS
Header photo: A report by the state insurance commissioner said Georgia health insurance companies offering major medical coverage did not submit sufficient 2022 information to be in compliance with state and federal mental health parity laws. (Credit: Jacob Lund)
Professionals still face licensing delays amid state’s transition to online system
The Gist Georgia’s professionals and business owners are still struggling to obtain professional licenses in a timely manner. As the Secretary of State’s Office rolls out its new Georgia Online Application Licensing System to expedite the process, the efficiency of this new process is being put to the test. What’s Happening Thursday morning at the …
Controversy over AP African American Studies class grows
Rashad Brown has been teaching Advanced Placement African American Studies at Atlanta’s Maynard Jackson High School for three years. He’ll continue to do so — even though the state’s top education official removed it from the list of state-funded course offerings for the upcoming school year. While Brown prepares to start teaching his class on …
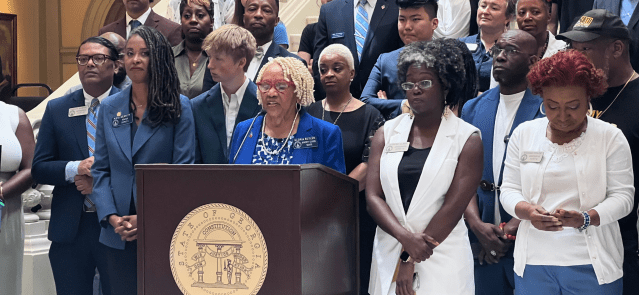
Students, teachers, lawmakers blast decision to end AP African American history classes
ATLANTA — A coalition of lawmakers, civil rights leaders, clergy, educators and students Wednesday called on the state’s education czar to rescind his decision to drop an advanced placement African American studies class from the state’s curriculum for the upcoming school year. “This decision is the latest attack in a long-running GOP assault on Georgia’s …
Kamala Harris’ presidential bid reinvigorates Georgia Democrats
Georgia Democrats have gained new momentum heading into the November election, propelled by President Joe Biden’s decision to bow out of his reelection bid and hand the reins to Vice President Kamala Harris. The historic decision, announced Sunday, is expected to prove pivotal in the national and state political arenas and breathe new life and …