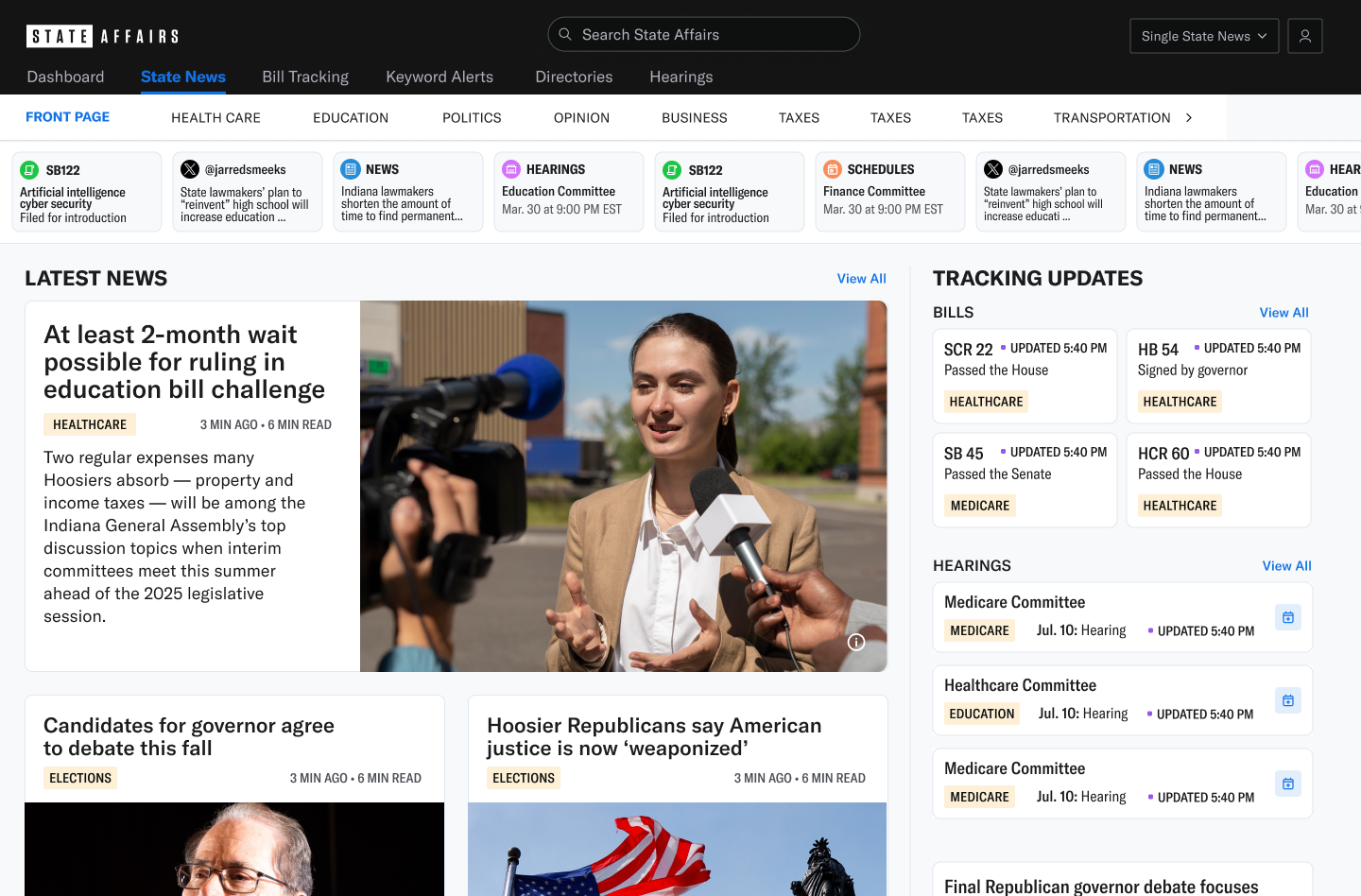
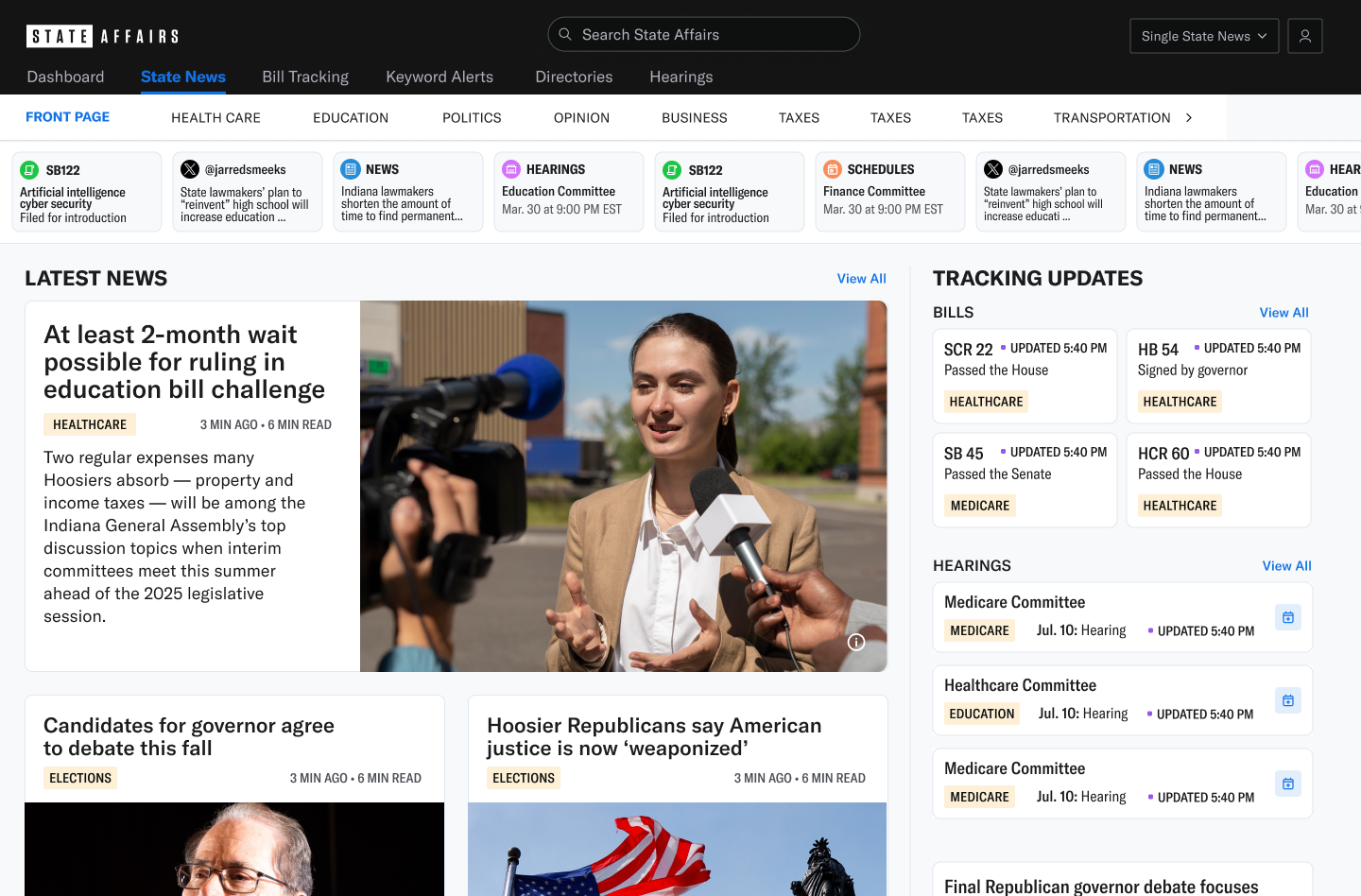
State news and AI-powered policy intelligence—personalized, nonpartisan, on-the-ground, and built for those who act first.






Trusted by thousands of organizations across the United States






























%201.png)










%201.png)










Original nonpartisan reporting. Nationwide reach. Unmatched legislative depth.




Our Local, Nonpartisan Statehouse News Brands


























See how our AI-tuned tools help individuals, teams, and organizations stay ahead of policy change.