Stay ahead of the curve as a political insider with deep policy analysis, daily briefings and policy-shaping tools.
Request a DemoMobile program launched in Georgia to help Medicaid recipients keep coverage

A mobile unit operated by Eastchester Family services. It a retrofitted RV. (Credit: Tammy Joyner)
Georgia Medicaid recipients now have a mobile program geared to helping them keep their coverage.
CareSource Georgia is traveling the state in eight medically-staffed, retrofitted recreational vehicles to provide health care to Medicaid recipients and to ensure uninterrupted coverage continues without disruption.

“This initiative is part of our outreach to raise awareness about what Georgians can do to retain Medicaid coverage during the redetermination process,” said Jason Bearden, CareSource Georgia’s Health Plan president.
State officials use the redetermination process, also known as Medicaid unwinding, to decide who is eligible for the program and to remove those who no longer qualify. The process was halted during the pandemic, allowing many children and adults who normally would have been removed to continue getting coverage during the pandemic. Now that the pandemic has subsided, the removal moratorium has ended. The renewal process continues through May. Some 545,000 people in Georgia could lose coverage, according to state estimates.
What’s happening?
CareSource has teamed with various medical outlets to operate the fleet of RVs to provide medical services and help with the Medicare redetermination process through the Wellness on Wheels (WOW) program.
Borrowing from the days when doctors made house calls, Bearden said, WOW is “a community engagement initiative where we meet people where they are.”
The program enables Medicaid recipients to see doctors and medical staff in the RVs for primary care. During the visits, medical staff will ask recipients about their Medicaid eligibility and status and, if need be, help them update necessary information to make sure their Medicaid coverage continues.
Many Medicaid recipients in Georgia are unaware state officials are reviewing the eligibility status of the 2.7 million Medicaid recipients over the next year, Bearden said. CareSource officials want to help reach those Georgians.
“When we learned that redetermination was starting up, we embarked on a plan to say, ‘Hey, let’s leverage what we’re already doing. And let’s bring laptops and let’s bring iPads and let’s bring our team where members come in and they can engage, and they can redetermine and punch in their information right here on site,’” Bearden told State Affairs.
Why It Matters
The CareSource initiative comes at a time when many Medicaid recipients have recently lost coverage as state officials work to determine who is eligible for the program.
More than 170,000 Georgians have lost access to Medicaid coverage since the unwinding began in April, according to a Georgia Budget & Policy Institute blog. Nine out of 10 of those people lost it for “procedural reasons, which means they’re likely still eligible but are denied coverage due to a human or technological error in the renewal process,” GBPI researcher Leah Chan noted in the blog.

Georgians face an extra hurdle getting Medicaid. Georgia is the only state in the country that ties work requirements to Medicaid coverage. Georgia’s Pathways to Coverage program, which began July 1, requires low-income people to complete 80 hours of work, school or volunteering to qualify for the government benefit. So far, fewer than 300 people have signed up for Pathways, according to state data.
The company is deploying the fleet of WOW mobile medical vehicles throughout the state to help ensure people’s coverage is not disrupted during the unwinding process. They also want to help those who lose coverage regain it, if eligible.
CareSource has made 10 WOW stops since the program began in January, Dr. Minh Nguyen of CareSource told State Affairs.
“At each community visit, we provide food to the families, and back-to-school supplies for the kids,” Nguyen said. “We’ve had over 7,000 participants this year already, and we’ve provided 150 well-child visits to kids who normally didn’t get care.”
What’s Next?
Another 10 WOW stops are set for September and more statewide stops will be added through the rest of the year, according to Dr. Seema Csukas, chief medical officer at CareSource.
The 10 September stops are slated for metro Atlanta and possibly parts of Southeast Georgia and Southwest Georgia, Csukas said.

CareSource is a national nonprofit managed-care organization with over 2.3 million members. It administers one of the largest Medicaid managed-care plans in the nation and serves more than 500,000 Medicaid recipients in Georgia.
Have questions, comments or tips? Contact Tammy Joyner on X @lvjoyner or at [email protected].
X @StateAffairsGA
Instagram@StateAffairsGA
Facebook @StateAffairsGA
LinkedIn @StateAffairs
Header image: A mobile unit (a retrofitted RV) operated by Eastchester Family services stopped by the State Capitol. (Credit: Tammy Joyner)
Read more on Medicaid in Georgia:
Professionals still face licensing delays amid state’s transition to online system
The Gist Georgia’s professionals and business owners are still struggling to obtain professional licenses in a timely manner. As the Secretary of State’s Office rolls out its new Georgia Online Application Licensing System to expedite the process, the efficiency of this new process is being put to the test. What’s Happening Thursday morning at the …
Controversy over AP African American Studies class grows
Rashad Brown has been teaching Advanced Placement African American Studies at Atlanta’s Maynard Jackson High School for three years. He’ll continue to do so — even though the state’s top education official removed it from the list of state-funded course offerings for the upcoming school year. While Brown prepares to start teaching his class on …
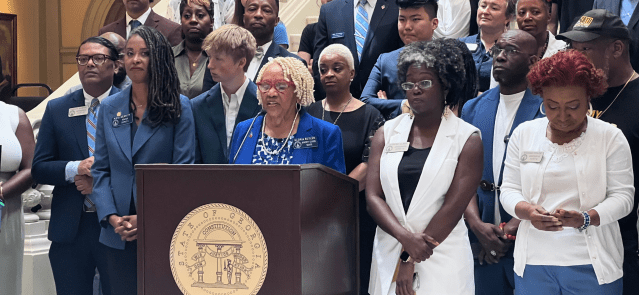
Students, teachers, lawmakers blast decision to end AP African American history classes
ATLANTA — A coalition of lawmakers, civil rights leaders, clergy, educators and students Wednesday called on the state’s education czar to rescind his decision to drop an advanced placement African American studies class from the state’s curriculum for the upcoming school year. “This decision is the latest attack in a long-running GOP assault on Georgia’s …
Kamala Harris’ presidential bid reinvigorates Georgia Democrats
Georgia Democrats have gained new momentum heading into the November election, propelled by President Joe Biden’s decision to bow out of his reelection bid and hand the reins to Vice President Kamala Harris. The historic decision, announced Sunday, is expected to prove pivotal in the national and state political arenas and breathe new life and …