Stay ahead of the curve as a political insider with deep policy analysis, daily briefings and policy-shaping tools.
Request a DemoHealth care providers and Gov. Kemp balk at proposed federal rule for staffing nursing homes

Header photo: Nursing homes in Georgia may be required to hire more registered nurses if a proposed federal rule goes into effect. (Credit: Rido)
The Gist
A proposed new federal rule mandating minimum staffing levels at nursing homes is causing consternation among Georgia’s senior care providers and health care advocates. Public comment on the rule ended this week, and Gov. Brian Kemp joined 14 other Republican governors in a letter to President Joe Biden asking him to reconsider what they call an unfunded mandate that could force many long-term facilities to close, “eroding health care for some of our most vulnerable citizens.”
What’s Happening
The federal regulations proposed by the Centers for Medicare and Medicaid Services on Sept. 1 would require long-term care facilities receiving federal funding to have a registered nurse on site 24 hours a day, seven days a week, and to staff their facilities with R.N.s a minimum of 33 minutes per resident per day, as well as provide staffing by nurse aides for another 2 hours and 27 minutes per resident per day.
A White House statement issued with the proposed rule said that “too many nursing homes chronically understaff their facilities — resulting in poor, substandard care that endangers residents. When nursing homes stretch workers too thin, residents may be forced to go without basic necessities like hot meals and regular baths, or even forced to lie in wet and soiled diapers for hours. Residents also suffer avoidable injuries like falls and bedsores. Workers become burnt out from the daily struggle to deliver the quality care they know their residents deserve.”
The U.S. Department of Health and Human Services seeks to set a federal floor for staffing levels “so that nursing home owners could not slash staffing to unsafe levels,” the White House said.
But many health care advocates say maintaining such staffing ratios will be impossible to achieve.
“Here’s the problem: There are no staff. We can’t find them,” said Chris Downing, CEO of the Georgia Health Care Association, adding that the minimum staffing mandate would require Georgia nursing homes to hire another 3,600 full-time employees (2,700 nurse aides and 900 R.N.s) at a time when the nursing industry is still hurting from staff lost during the COVID-19 pandemic.

Georgia’s skilled nursing industry “lost roughly 6,000 people during the pandemic, and we’re still trying to dig out from that,” Downing said. “Georgia already has one of the worst R.N.-to-patient ratios in the country,” with 750 registered nurses to 100,000 patients, he said.
The Georgia Health Care Association has asked why the new rule does not include in its required staffing formula licensed practical nurses, social workers, physical therapists and other members of multidisciplinary teams that routinely provide care at nursing homes.
“These professionals meaningfully improve the quality of care residents receive, yet CMS’s [Centers for Medicare and Medicaid Services] proposed regulations totally ignore these contributions,” the governors’ letter to Biden last week stated. “Indeed, CMS’s own industry study found that there was no discernable [sic] difference in the quality or safety of LPN-provided care compared to R.N.-provided care.”
Why It Matters
A study by the American Health Care Association and national accounting firm CliftonLarsenAllen found that 76% of 353 Georgia nursing homes are not meeting at least one of the three proposed staffing requirements, and less than 1% of nursing homes in the state are meeting all three of the proposed requirements.
If nursing homes can’t increase their workforce to the mandated levels, the study projects that as many as 9,600 nursing home residents in Georgia could be displaced.
“If they can’t comply with the requirements, then naturally they’re going to stop accepting patients so they can get a manageable census, which may mean shutting a wing down, or in some cases closing a whole facility,” said Downing.
The study also estimated that the staffing mandate would cost nursing homes in the U.S. $6.8 billion and those in Georgia $187 million annually to implement, at a time when low Medicaid reimbursement rates for nurses already make budgeting and hiring difficult.
The Biden Administration also announced a plan to invest $75 million in a “national nursing career pathways campaign” providing tuition support to recruit, train and transition workers into nursing home careers, but health care advocates said significantly more investment is needed.
What’s Next
The Centers for Medicare and Medicaid Services has received more than 40,000 comments from the public and will have to review and respond to them before finalizing the rule. The staffing requirements in the rule, if it stands, would be phased in over three years for urban facilities and five years for rural facilities, which have more challenges hiring health care workers.
Critics of the proposed rule say that extended timeline won’t help, as the staffing shortage among nurses is predicted to get worse over the next several years.
According to a study by the National Council of State Boards of Nursing, 100,000 R.N.s left the workforce during the pandemic. The council also estimates that another 800,000, or one-fifth of R.N.s in the U.S., intend to leave the profession by 2027 due to stress, burnout and retirement.
“We’re sympathetic to both sides of the argument,” said Vicki Johnson, chair of the Georgia Council on Aging. “Seniors in long-term care facilities are better protected with adequate staffing requirements to meet the needs of residents, yet we also understand what a predicament the providers are in because of the limited number of employees, particularly R.N.s, that are available.”
Johnson said the council would like to see more done “to enhance the pipeline to attract students to the nursing profession. We’d like the state to dedicate more resources to that, and also give more flexibility for on-the-job training, in order to help recruit and retain nursing staff.”
Read these related stories:
Have questions, comments or tips on health care in Georgia? Contact Jill Jordan Sieder on X @journalistajill or at [email protected].
X @STATEAFFAIRSGA
Facebook @STATEAFFAIRSGA
Instagram @STATEAFFAIRSGA
LinkedIn @STATEAFFAIRS
Header photo: Nursing homes in Georgia may be required to hire more registered nurses if a proposed federal rule goes into effect. (Credit: Rido)
A primer on the Nov. 5 ballot measures: What you need to know
In addition to voting for president and down-ballot candidates in the Nov. 5 election, Georgians will decide on a couple of tax measures and whether to create a statewide tax court. Three questions call for a statewide vote, all of which appear at the end of the ballot. The first time most voters see these …
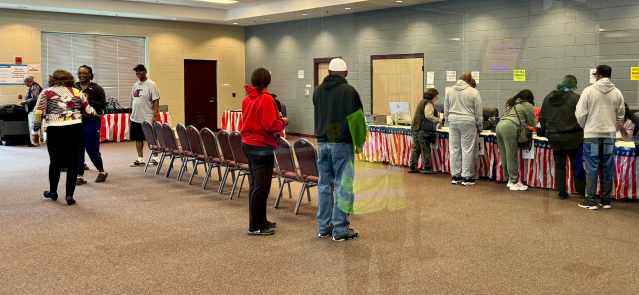
Tuesday’s early voting turnout sets highest 1-day record in a presidential election year
More than 306,000 Georgians voted on the first day of early voting Tuesday, setting the highest one-day early voting turnout in a presidential election year. Tuesday’s statewide turnout of 306,118 voters more than doubled that of first-day early voting for the general election four years ago, state election officials reported just after 8:30 p.m. Tuesday. “It’s …
Georgia Supreme Court restores state’s 6-week abortion ban
The Georgia Supreme Court reinstated the state’s six-week abortion ban Monday, a week after a lower court judge overturned the controversial measure. The court ordered the stay while it considers the state’s appeal of the lower court ruling. The head of an anti-abortion organization praised the Supreme Court’s decision, which went into effect at 5 …
Weekend Read: Georgia abortion clinics see surge after 6-week abortion ban struck down
While Georgia lawmakers seek to restore the state’s six-week abortion ban struck down earlier this week, some abortion clinics are reporting increased activity as women seek help during what some view as a temporary reprieve in the state law. Fulton County Superior Court Judge Robert McBurney on Monday struck down Georgia’s abortion ban, ruling it …