Stay ahead of the curve as a political insider with deep policy analysis, daily briefings and policy-shaping tools.
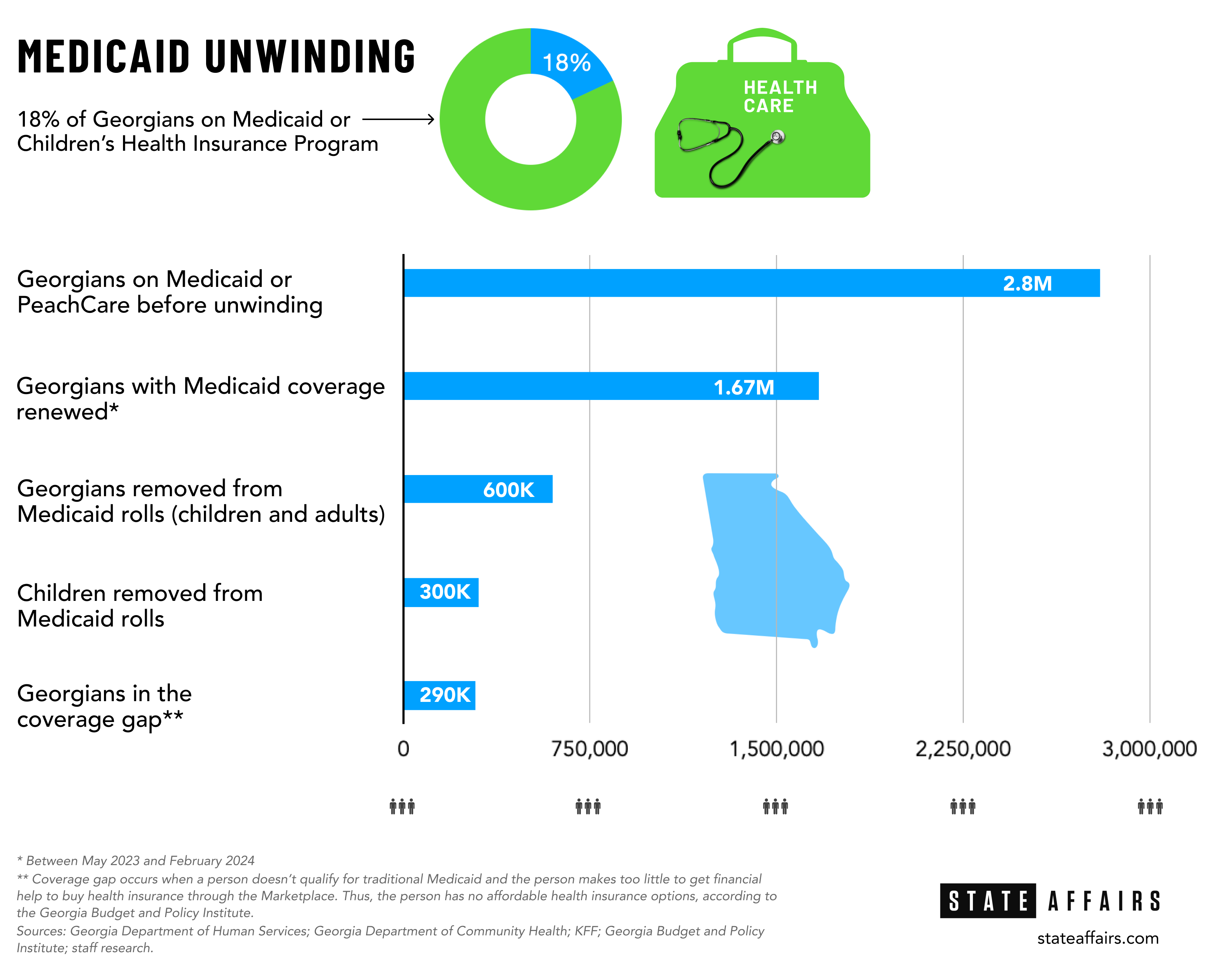
Request a Demo600K dropped from Medicaid; half are children
(Design: Brittney Phan)
- Children account for half of Georgians being removed from Medicaid
- Georgia’s Medicaid eligibility review process is fraught with problems
- Streamline and do more automatic renewals, experts say
Editor’s note: This is the first in a two-part series looking at two Medicaid-related topics in Georgia — “Medicaid unwinding” and Pathways to Coverage. To read Part 2 on Pathways, go here. Pathways is Georgia’s work-for-Medicaid alternative to expanding Medicaid. This story looks at the Medicaid unwinding process.
The Gist
More than a year into Georgia’s efforts to sort out who keeps and who no longer gets Medicaid coverage, roughly 600,000 people have been ousted — half of them children.
And it’s not over yet.
The eligibility review process better known as Medicaid unwinding officially ended in Georgia in May, but state officials are still plowing through. Medicaid unwinding is the nation’s largest health coverage event since the Affordable Care Act — aka Obamacare — was rolled out in 2013.
Red tape, along with procedural and technical glitches, has made an arduous task even more of an administrative burden for state agency workers and Medicaid recipients, Medicaid experts say.
“The Medicaid unwinding process has highlighted how difficult it is for families to navigate the Medicaid eligibility review process,” Callan Wells, senior health policy manager for the Georgia Early Education Alliance for Ready Students, told State Affairs. “While the past year has drawn attention to these arduous annual reviews, the reality is families struggled through this process before the pandemic and will continue to do so after the unwinding.”
What’s Happening
As of June 14, more than 23 million Medicaid recipients nationwide have been removed from the rolls and nearly 51 million have had their coverage renewed through the unwinding process, according to health research organization KFF, which has collected data on all 50 states and the District of Columbia.
Medicaid helps people who can’t afford medical care pay for some or all of their medical expenses. The program is administered by the Georgia Department of Community Health and pays medical expenses using state and federal money.
Nearly 7 in 10 people removed from the rolls had their coverage terminated for procedural reasons, meaning they didn’t complete or didn’t understand the renewal process or the state had outdated information on them. As a result, many might still be eligible.
In Georgia, 78% of those people were removed due to procedural issues while 22% were deemed ineligible, according to KFF data.
Another organization looking at Georgia’s Medicaid unwinding performance — Georgetown University’s Center for Children and Families, a nonpartisan policy and research center — found that Georgians were being removed from the Medicaid rolls at a higher rate than the rest of the country.
The center, which did a state-by-state analysis of Medicaid unwinding enrollment, also found that between May 2023 and March 2024, 32% of Medicaid recipients in Georgia had had their coverage automatically renewed. The national average was 43%, the report noted.
“Georgia is behind,” Joan Alker, a Georgetown research professor and the center’s executive director and co-founder, told State Affairs.
Beyond the numbers is growing concern about the future effect unwinding will have on Georgians, especially children. As it stands, 1 in 5 children who had health plan under Medicaid may be going without coverage, experts noted.
“Unfortunately, Georgia has been a leader in disenrolling children from Medicaid. In a state like Georgia, which has not expanded Medicaid, this has become a children and maternal health issue,” Alker said. “If a child breaks an arm, it exposes the family to medical debt. It prevents children from getting the care they need to grow and thrive. Conditions like asthma get worse.”
Why It Matters
Medicaid unwinding began in April 2023 as a way to renew recipients’ coverage. It was also intended to cull hundreds of thousands of recipients who were eligible to stay on the federal-state health coverage during the COVID-19 pandemic but now no longer qualify.
“This is historic,” Leah Chan, director of Health Justice at Georgia Budget and Policy Institute, told State Affairs. “Because of that pandemic-era policy, everybody got to keep their coverage during the pandemic, and then every single man, woman and child
had to have their [Medicaid] eligibility redetermined. I’m not sure that there has ever been a time like this.”
State officials have their work cut out for them:Determining the eligibility of about 2.7 million adults and children is like unraveling a big ball of tangled Christmas lights. Because of Georgia’s stringent eligibility rules, it’s tough for many adults to get Medicaid. Nearly 7 in 10 Georgians receiving Medicaid are children.
“We are seeing too many people losing coverage because of administrative red tape, and there are a concerning number of children,” Chan said. “We don’t know if those children have regained coverage or are under a different form of insurance.”
State officials overseeing the unwinding process aren’t forthcoming except to say 1.67 million Georgians had their Medicaid coverage renewed between May 2023 and February 2024. That’s the latest data available from the Georgia Department of Community Health, which is overseeing the process.
“Our members whose redetermination requests are still pending are continuing to receive services until their respective requests have been completed,” department spokesperson Fiona Roberts said in a statement to State Affairs.
Efforts to reach the department’s commissioner, Russel Carlson, were unsuccessful.
But experts say Georgia’s Medicaid unwinding process is plagued with bureaucracy, long wait times, technical glitches and a short-staffed and overburdened department. In February, for example, 4 in 10 renewal applications took longer than the 45-day deadline to process, according to Jennifer Wagner, director of Medicaid eligibility and enrollment for the Center on Budget and Policy Priorities, a Washington, D.C.-based nonpartisan think tank.
“Georgia has a fairly high rate of procedural denials, which is essentially folks who are losing coverage, and they may likely still be eligible, but they’re losing it for some sort of human error or technological error,” Chan said. “That procedural denial rate has stayed fairly elevated through the months of data that are available, and that is concerning.”
Several concerns have emerged during the yearlong process:
- Children bearing the brunt. About 300,000 children have been removed from the Medicaid rolls so far. That’s the third-worst child health care disenrollment rate in the country, according to the Georgetown University report.
- A slow, arduous application process. For instance, 40% of renewal applications in February exceeded the 45-day processing deadline, according to Wagner. “A lot of those applications are from people who lost coverage at renewal,” Wagner said. “It’s not all people who are newly eligible for Medicaid. It’s people who got cut off at renewal because they didn’t get the form. Something happened during the process.”
- Other bureaucratic hassles. Over 500,000 Georgians were kicked off Medicaid in February, the latest data available, due to missing paperwork. Health research organization KFF found 8 in 10 Georgians who’ve lost Medicaid coverage were removed for missing paperwork, putting Georgia among the 10 worst states in the nation for Medicaid disenrollment.
- Technical glitches. Medicaid recipients with only smartphones to access Medicaid services through the Georgia Gateway website were hampered by glitches in the system and misleading or contradictory information, according to The Atlanta Journal-Constitution.
- Overwhelmed, underpaid staff. Even with hundreds of additional hires, the head of the state agency responsible for Medicaid unwinding told lawmakers earlier this year the department was overwhelmed and understaffed. Some offices could be open only three days a week instead of five because they didn’t have anyone to run them. Medicaid recipients looking for help have reported finding caseworkers’ voicemail boxes full and little to no guidance, experts say.
“They have tried to, in some ways, address pay and they’ve tried to hire more folks,” Chan said. “But there’s just not enough people, not enough pay and there’s just too much work to go around. The whole system is built on these two things — the frontline caseworkers and the technology — and both of those things we have not paid enough attention to, and I think that has revealed itself during the Medicaid unwinding.”
What’s Next?
Georgia is one of 10 states that hasn’t expanded Medicaid, so those who are being kicked off the rolls face an additional hurdle finding affordable health care. States that have not expanded Medicaid have double the rate of uninsured people — 14.1% vs. 7.5% — compared with states that expanded Medicaid, according to KFF.
Those who fall through the health care gap generally are Georgians between the ages of 18 and 40; people in rural areas and other places where higher-paying jobs are scarce; workers in low-paying fields such as food service, grocery, retail and child care; people with mental health and substance abuse conditions; and people of color. Blacks and Latinos account for half the people in Georgia’s Medicaid coverage gap, according to Laura Colbert, executive director of Georgians for a Healthy Future, an Atlanta-based nonprofit consumer advocacy group.
Here’s what experts say Georgia officials could do to make the process more efficient:
- Streamline the automatic renewal process. “Increasing the ex parte (automatic renewal) rate is key,” Wagner said. Ex parte involves Medicaid eligibility workers using reliable data such as the Supplemental Nutrition Assistance Program (SNAP) to verify and confirm Medicaid recipients’ eligibility. That helps cut procedural terminations and speed up the process. The KFF report showed that all states made changes to simplify or streamline the renewal process and they want to keep many of the changes after unwinding ends.
- Improve communication with Medicaid recipients. What do the Medicaid renewal notices look like? Are they going to the right addresses? Are they clear and easy to understand?
- Address delays in timely application processing. “It’s very complicated,” Wagner said. “And the fact that their application processing timeliness is so bad and deteriorating says to me that [state workers] aren’t returning phone calls, that it’s a long wait time for a call center at an office. It usually means that kind of assistance is melting down a little bit.”
- Modify the process so staff can keep up with the workload. Answer questions. Return phone calls. Provide guidance and customer service.
- Create outreach and enrollment programs. That will help reclaim some of the children who’ve been removed, Alker said. Since August, CareSource has traveled throughout Georgia in medically staffed vehicles to provide health care to Medicaid recipients and help them through the unwinding process. The company also has gone to YMCAs, churches, grocery stores and Walmarts to get the word out, president Jason Bearden said. “That has been a great success,” he said. CareSource administers one of the largest Medicaid managed-care plans in the nation and serves more than 500,000 Georgia recipients.
- Expand Medicaid. “That’s the single most impactful thing you could do, especially for this population we are talking about in Georgia,” Wagner said.
Learn more about the Medicaid redetermination process, known as Medicaid unwinding, here and here.
Surf the Medicaid Enrollment and Unwinding Tracker here.
Have questions, comments or tips? Contact Tammy Joyner on X @lvjoyner or at [email protected].
Newly minted Senate Minority Leader Harold Jones II: ‘I’m not the typical back-slapping politician’
Nearly 10 years into legislative life, Sen. Harold Jones II wouldn’t change anything about the experience. “I love every minute of it. Even when I hate it, I love it,” the 55-year-old Augusta Democrat told State Affairs. Come January, Jones will add another role to his legislative duties: Senate minority leader, a job held for …
Gov. Kemp calls on state agencies to be fiscally restrained amid record $16.5B surplus
The Gist Gov. Brian Kemp asked the state’s 51 government agencies for continued fiscal restraint when drafting their amended fiscal year 2025 and 2026 budgets. Most agencies adhered to his request even as the state’s general fund surplus hit a record $16.5 billion last month. Forty-five agencies, excluding state courts, followed the governor’s instructions to …
Georgia defies bomb threats as election chief declares a “free, fair and fast” vote amid record turnout
ATLANTA – Despite dealing with over 60 bomb threats, Georgia’s election chief said Tuesday the state’s general election went smoothly. Georgia had a record turnout with nearly 5.3 million people voting, Secretary of State Brad Raffensperger told reporters. Election officials in the state’s 159 counties have until 5 p.m. to certify votes. “We had a …
In the (state)house: Meet the newest members of the Georgia legislature
When lawmakers reconvene at the state Capitol on Jan. 13, there’ll be a cadre of new faces in the 236-member Georgia General Assembly, one of the nation’s largest state legislatures. All 236 statehouse seats were up for election this year. Most candidates ran unopposed. Incumbents in contested races easily kept their seats, with the exception …




