Stay ahead of the curve as a political insider with deep policy analysis, daily briefings and policy-shaping tools.
Request a DemoWill reducing prior authorization help or hurt the state’s health care system?

(Credit: Maudib)
When Dr. Elizabeth Struble thinks a patient has a kidney stone, she often sends them home with some medication and contacts insurance to order a CAT scan.
But it can take insurance providers up to five days to approve the scan. Meanwhile the patient’s symptoms can continue to worsen, and eventually some patients might need to be admitted to a hospital because they became ill or septic.
“This is a common story, ” the family medicine doctor from North Manchester said during a committee hearing on the bill. “This happens all the time.”
Struble and other physicians say delays due to prior authorization requirements — when health care providers need to obtain approval from insurance companies before issuing care — are limiting their ability to treat patients quickly and properly. However, insurers say nixing prior authorization requirements could increase unnecessary procedures and, as a result, health care costs.
Indiana lawmakers are grappling with those conflicting messages while they consider Senate Bill 3, which would significantly restrict when insurance providers can require prior authorization for medical care.
“The original idea behind prior auth was that it could contain health care costs,” said bill author Sen. Tyler Johnson, R-Leo. “What we see every day is that prior authorization has become a huge hurdle to patients getting the care they need.”
The proposal has passed out of one legislative committee but must clear one more before the full Senate can vote on it.
In a testament to the complexity of the debate, the bill was pulled from the Senate Appropriations Committee calendar Thursday over concerns that decreasing prior authorization requirements could fiscally impact the state, Senate President Pro Tem Rodric Bray said.
“We’ll take a look at that,” he said, “and hopefully get to the hearing next week.”
What Senate Bill 3 does
Under Senate Bill 3, insurance providers could not require prior authorization for emergency services — such as when someone needs their appendix removed — routine care and prescription drugs.
It would also prohibit insurance companies from requiring prior authorization on more than 1% of services and give health care providers a yearlong break from prior authorization requirements if their prior authorization approval rating the previous year was above 80%.
That so-called gold card policy is similar to those passed in West Virginia, Texas and Louisiana.
The procedures or drugs that still would require prior authorization would need to be reviewed by a physician, meaning insurance companies couldn’t use just a computer algorithm to decide who doesn’t get care.
“The patient needs to be at the center of this discussion,” said Johnson, an emergency room physician. “It’s really easy to see that [prior authorization] puts a big burden in front of a patient getting care, and that’s a huge administrative cost.”
So what would reducing prior authorization mean on a practical level for Hoosiers?
It could help those who have kidney stones or need physical therapy.
Jason Hazelett, the owner of Steppin’ Up Physical Therapy in Fort Wayne, said he had a patient whose leg was partially amputated and was ready to begin therapy after getting a prosthetic leg so that he could relearn how to walk. Throughout physical therapy, Hazelett’s company had to keep seeking prior authorization for additional physical therapy sessions, leading to long gaps in care.
“This gentleman is getting set back during that time there was no therapy,” Hazelett said, ”not because we couldn’t see him, but because we were waiting on a peer review or prior authorization to come back.”
Dr. Elizabeth Wright, chief ambulatory officer at Hendricks Regional Health, brought up another scenario in which a patient had severe lower back pain. She said the patient needed advanced imaging, but because she had to seek prior authorization first, that care was delayed.
“That delay led to chronic pain which could have been prevented if we had initiated treatment sooner,” Wright said. “These are things that we run into every day.”
She added that her office staff spends hours daily working on prior authorizations.
It’s not just an Indiana concern. According to a 2022 American Medical Association survey, 33% of physicians reported that prior authorization has led to “a serious adverse event” for one of their patients.
Does prior authorization increase or decrease health care costs?
Insurance providers and business representatives often say that prior authorization helps keep health care costs lower. But it’s unclear whether a net economic benefit to prior authorization exists.
A 2019 report from Altarum’s Center for Value in Health Care found that studies show mixed results on the impact of prior authorization. There’s been no combined cost-benefit analysis, the report authors said.
“[Prior authorization] can reduce avoidable care while helping to control health care expenditures,” the report authors wrote. “On the other hand, the process imposes time and cost burdens, can result in delays in needed care, and causes confusion and often frustration for providers and patients.”
The Indiana Chamber of Commerce and the Indiana Manufacturers Association opposed Senate Bill 3 over concerns it could increase health care costs for businesses.
“Let’s not mistake the occasional hiccup that we’ve heard about today as a problem with the system’s fundamental value,” Ashton Eller, vice president of health care policy and employment law for the Indiana Chamber of Commerce, said during a committee hearing on the bill. “The prior authorization process is a tool in the employer’s toolbox to help contain health care costs.”
A legislative fiscal analysis of the bill warns that the state — an employer itself — could have to pay more money if a decrease in prior authorization leads to state employees or Medicaid users accessing more medical care.
Blaire Hadley, director of government relations for Insurance Institute of Indiana, said her organization is open to discussing strategies for improving prior authorization but emphasized that the tool ensures patients get the right care at the right time in the right place.
“We know this process is not perfect,” Hadley said. “However, we are committed to working with all of you and with the market, with providers and hospitals, while also keeping in mind what our employer partners are asking for.”
What’s next?
Like most legislation targeting health care costs, the bill faces strong opposition and could be challenging to push across the finish line. The business community and those in the health insurance industry — both powerful lobbying groups at the Statehouse — have concerns about the legislation.
Last year many of Republicans’ attempts to pass meaningful bills targeting health care costs were watered down before their final passage.
The deadline for the bill to make it out of the Senate Appropriations Committee is Thursday. A committee agenda for this week has not been released yet.
Contact Kaitlin Lange on X @kaitlin_lange or email her at [email protected].
Facebook @stateaffairsin
Instagram @stateaffairsin
LinkedIn @stateaffairs
4 things to know about Braun’s property tax proposal
Sen. Mike Braun, the Republican candidate for Indiana’s governor, released a plan for overhauling property taxes Friday morning that would impact millions of Hoosiers, Indiana schools and local governments. “Nothing is more important than ensuring Hoosiers can afford to live in their homes without being overburdened by rising property taxes driven by rapid inflation in …
Bureau of Motor Vehicles looks to add new rules to Indiana’s driving test
The Bureau of Motor Vehicles wants to amend Indiana’s driving skills test, putting “existing practice” into administrative rule. Indiana already fails drivers who speed, disobey traffic signals and don’t wear a seatbelt, among other violations. Yet the BMV is looking to make the state’s driving skills test more stringent. A proposed rule amendment looks to …
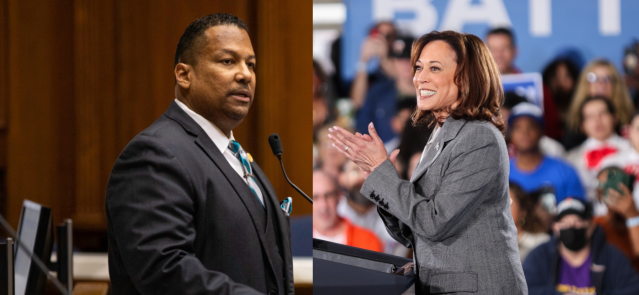
In Indianapolis, Harris says she’s fighting for America’s future
Vice President Kamala Harris, the presumptive Democratic presidential nominee, told a gathering of women of color in Indianapolis on Wednesday that she is fighting for America’s future. She contrasted her vision with another — one she said is “focused on the past.” “Across our nation, we are witnessing a full-on assault on hard-fought, hard-won freedoms …
Indiana Black Legislative Caucus endorses Harris, pledges future support
The Indiana Black Legislative Caucus unanimously voted Wednesday to endorse Vice President Kamala Harris’ presidential run and will look at ways to assist her candidacy, the caucus chair, state Rep. Earl Harris Jr., D-East Chicago, told State Affairs. The caucus is made up of 14 members of the Indiana General Assembly, all of whom are …